What You Need to Know: Exciting Changes to Ohio’s Medicaid Program Starting on Oct. 1
Date: 10/01/22
On October 1, 2022, Ohio Medicaid implemented exciting improvements for members and providers!
What Buckeye Health Plan Ohio Medicaid Members Need to Know:
Pharmacy benefits for Medicaid managed care plans are now covered through Gainwell Technologies, Ohio Medicaid’s single pharmacy benefit manager (SPBM).
If you have questions about your pharmacy benefits, call the Gainwell Customer Support Center at (833) 491-0344, 24 hours a day, 7 days a week. You also can email Gainwell Customer Support or visit the Gainwell SPBM website.
You should begin using the new Next Generation Ohio Medicaid managed care member ID card <Insert MCE name> recently mailed to you. The new card can be used for all your pharmacy or healthcare needs.
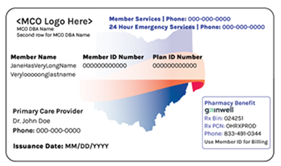
Sample image of the new Next Generation Ohio Medicaid managed care member ID card
If you haven’t received your new member ID card, you can still have prescriptions filled. Please bring your old ID card with you to your pharmac-y and contact Buckeye Health Plan at 1-866-246-4358 to learn more about how to print your card or access an electronic version.
Ohio Medicaid managed care members are encouraged to visit the Ohio Department of Medicaid website for additional resources and information about the latest launch of Ohio Medicaid’s Next Generation program.
What Ohio Medicaid Providers Need to Know:
All provider enrollment applications are now submitted using Ohio Medicaid’s new Provider Network Management (PNM) module. Providers access the module using an OH|ID login. The PNM module is the single point for providers to complete provider enrollment, centralized credentialing, and provider self-service. For resources and more information, visit Ohio Medicaid's Credentialing website.
Also effective October 1, Ohio Medicaid’s SPBM, Gainwell Technologies, began providing pharmacy services across all managed care plans and members.
- Pharmacy Claims: Providers should submit pharmacy claims for managed care members to Gainwell. Claims for fee-for-service members will continue to be submitted to the Fee-for-Service Pharmacy Benefit Administrator (PBA), Change Healthcare.
- Pharmacy Prior Authorizations: Gainwell will accept prior authorizations submitted through the electronic medical record (if supported), fax, phone, secure portal, and mail. Even if initiated prior to October 1, all Ohio Medicaid managed care members’ active pharmacy prior authorizations will be honored through their original expiration date.
For additional information related to Ohio Medicaid managed care pharmacy claims, prior authorization (including prior authorization forms and clinical criteria) and resources and training on how to utilize the SPBM portal, visit Ohio Medicaid's SPBM website.
Help desks are available to assist providers:
- If you have questions related to pharmacy claims, prior authorizations, and other pharmacy-related administrative tasks, contact the Gainwell SPBM Help Desk at (833) 491-0344 or email the Gainwell Customer Support Center at OH_MCD_PBM@GainwellTechnologies.com.
- Questions related to Centralized Credentialing and the PNM module, OH|ID, and portal password support should be directed to the Ohio Medicaid Integrated Help Desk (IHD) at (800) 686-1516 or email IHD@medicaid.ohio.gov.

